What Comes After WHO: The push to eradicate malaria
A 2025 policy recommendation from the World Health Organization (WHO) for malaria prevention ignites hope for ending one of humanity’s oldest diseases, but there’s still much to do.
According to the latest World Malaria Report, malaria directly affects over 280 million people every year, claiming an estimated 610,000 lives. In fact, between 2023 and 2024, there was an increase in nearly 9 million cases, mainly in the WHO Africa region. For a mother in endemic areas, the fear and grief of losing a child to a mosquito bite still exists.
Yet despite that fear, there is hope. Over the last decade, growing numbers of partners and resources have rapidly expanded malaria control efforts to the point where eradication feels attainable. Experts even believe it could be wiped out by 2050 if we pair existing tools with new innovations1.
In August 2025, the WHO endorsed spatial repellents as a new weapon in the fight against malaria, making them one of the first new categories of vector control tools to receive a policy recommendation from the WHO for malaria prevention within the last 25 years. Spatial repellents are easy to use, low-cost, long-lasting, and most importantly, effective. Studies show that using them properly can cut disease risk by up to 33 percent. SC Johnson’s Guardian™ spatial repellent provides protection for up to a year.
Now that policy approval has opened the door, the real challenge begins – making sure the right tools reach the people who need them most.
So how do we make that happen and take another step closer to eradication? SC Johnson is focusing on three key areas of implementation to help get there:
Building Local Capacity
There is a saying in global health: “The last mile is the hardest.” In many malaria-endemic areas, that last mile can literally mean walking miles upon miles for hours to reach the nearest clinic or relying on community volunteers for care. It’s not lack of care that holds back progress; it’s lack of access.
To help address this, SC Johnson is leveraging partnerships with global health organizations and public health channels, such as The MENTOR Initiative and Society for Family Health Rwanda, which have in-depth knowledge of these communities. These partners have helped the company establish 84 health clinics across Rwanda, Tanzania, South Sudan and Indonesia, reaching over one million people each year.

Sustainable progress also depends on the people who power local health systems. In many communities, women often fill this role informally. They handle more than half of all malaria cases, usually without pay or recognition. It also typically removes them from school or work, which can limit income opportunities. To help change that, SC Johnson partnered with the Society for Family Health Rwanda and the Rwanda Ministry of Health to establish a Certified Care educational program that trained and certified 10,000 Community Health Workers. It’s an important investment because, without ongoing support, these female health workers face burnout, and communities risk losing hard-won gains.
Driving Partnerships & Advocacy
Eradicating a disease depends not just on new ideas, but on alignment among a host of policy, funding, research, distribution and industry partners to work together broadly and collectively address the underlying causes of diseases and the barriers to prevention.
Even with the WHO’s approval, national health ministries must formally include new tools, such as spatial repellents, in their malaria control plans to unlock further funding. SC Johnson has been advocating alongside several governments to make this happen. Recently, Uganda, a country with a high malaria rate, became one of the first to include spatial repellents in its national strategy for 2026–2030.
Additionally, soon after the WHO’s announcement, SC Johnson convened health leaders to explore how Guardian could be deployed where malaria is most prevalent. They discussed how their countries could take the next steps to officially approve and register the product, make it available through public health programs and use it in endemic areas. Those conversations are already helping speed up registration, funding and distribution.

Scaling Up and Optimizing Manufacturing
The effort doesn’t end with discovery or policy; it depends on inventory and delivery. Real impact starts when these tools reach a family’s doorstep.
Locating production in regions where diseases like malaria and dengue are most prevalent brings manufacturing closer to the people who need protection, reduces costs, shortens supply chains and strengthens local economies in the process.
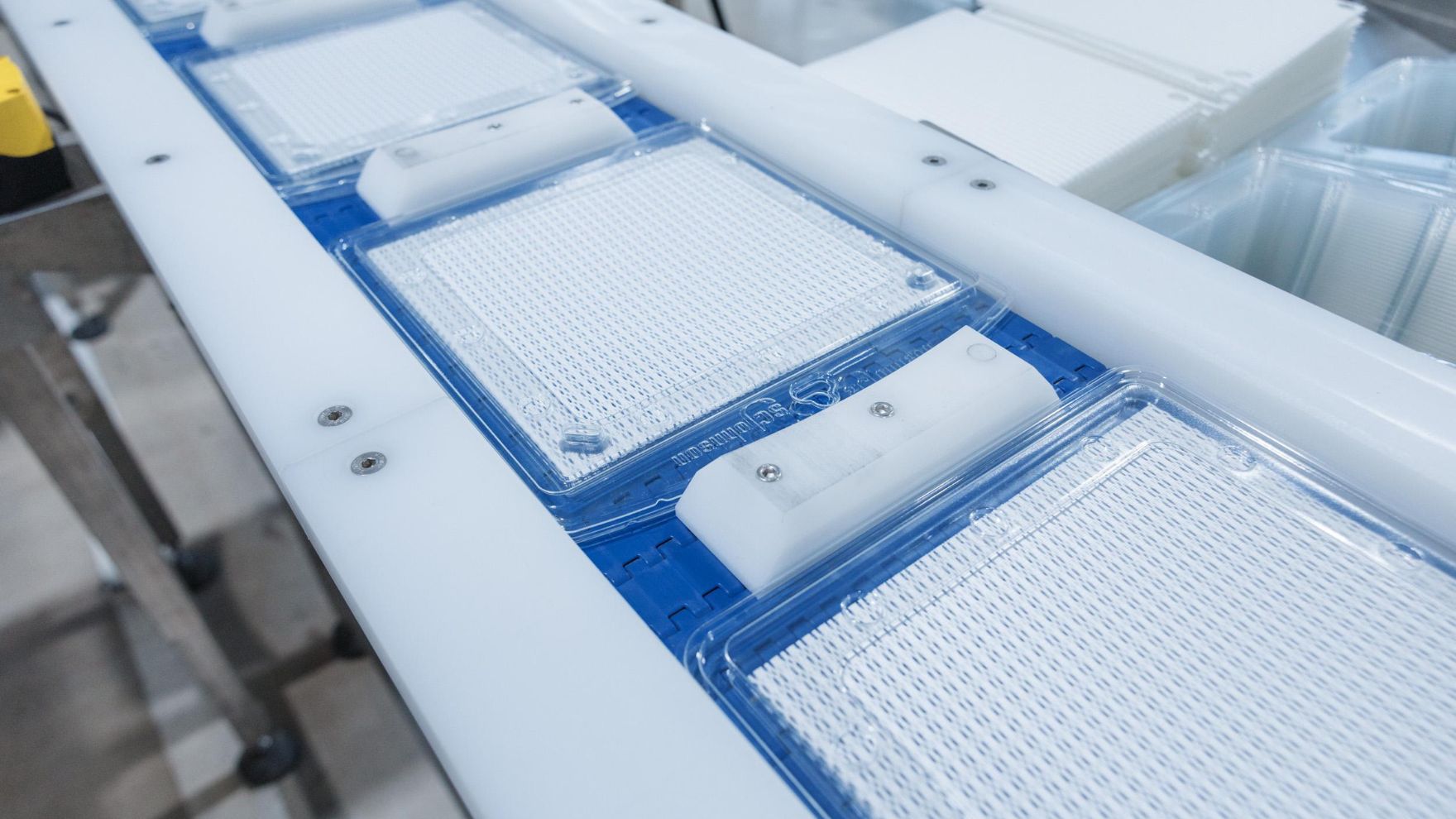
To meet growing demand, SC Johnson launched two new high-speed manufacturing lines at its Nairobi, Kenya, facility, capable of producing 20 million units annually. Another expansion is planned in Pilar, Argentina, in 2026.
The Road Ahead
Eradicating malaria won’t happen overnight, but every clinic built, every worker trained and every family protected adds up. Together, they move us toward something bigger: a world where no child dies from a mosquito bite and where disease eradication is not just a dream for future generations but a measure of how many lives are never lost in the first place.
